What is Pleurisy?
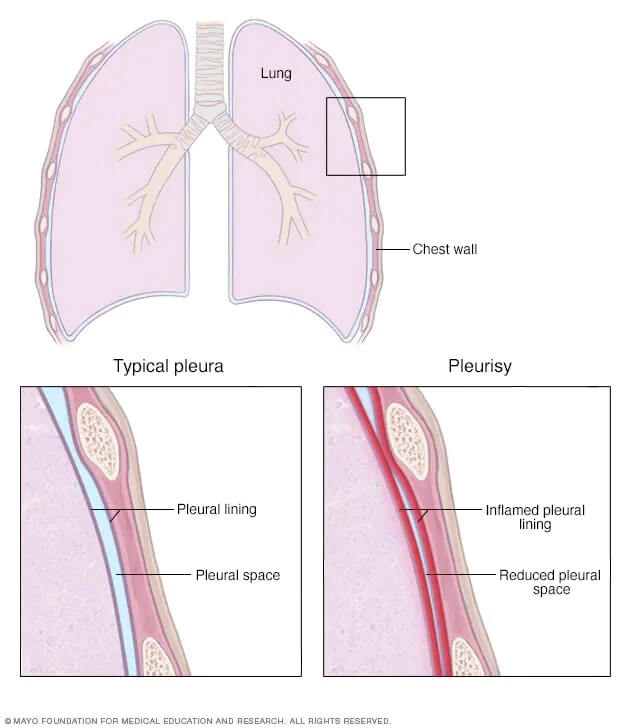
Pleurisy is the agitation of the pleural surfaces through friction. Our lungs are covered by a close fitting, thin lining called the visceral pleural. A second thin lining, called the parietal pleura, covers the inner wall of our chest cavity. Between these 2 layers is a small amount of pleural fluid to reduce friction as the two surfaces move against each other during breathing.
Pleurisy describes the sharp chest pains that results from inflammation of the pleural layers. This can occur from a decrease in the pleural fluid causing friction between the two surfaces. Conversely, an increase in pleural fluid can excessively separate localised sections of the pleural layers causing uneven movement. There may also be existing inflammation of the pleural layers from another underlying condition.
Some of the underlying conditions that can lead to pleurisy include:
– Infections (either viral or bacterial)
– Autoimmune disease
– Malignant tumours
– Direct physical trauma
– Inhalation or exposure to caustic substances, such as chemicals or drugs
– Various respiratory conditions
A doctor can confirm a diagnosis of Pleurisy following a detailed investigation of your symptoms, medical history and using specific tests to rule out other possible conditions.
Common signs and symptoms specific to pleurisy include:
– Shallow breathing – often rapid to compensate for lack of volume
– Wheezing – if sufficient lung capacity is impeded
– Coughing – can be painful or sputum productive if underlying infection is present
– Pain with deep breathing and thoracic expansion
What can physiotherapy treatment for pleurisy involve?
Subjective:
A discussion between you and your physiotherapist to find out what symptoms you are experiencing, and how your condition is affecting your lifestyle and activities of daily living (ADLs)
Objective:
An assessment to discern the presence of any pain, your current breathing pattern, respiratory rate, lung volume and a series of special tests to identify the presence of any mucus retention and lung function impairment.

Treatment:
A specialised treatment plan can be devised by your physiotherapist based on their findings above. Depending on the severity of your condition, treatment may include:
Secretion clearance
- Effective/productive coughing techniques
- Postural drainage positioning and advice
- Manual assistance – including percussion and vibration
Breathing techniques:
- Controlling respiratory rate
- Diaphragmatic breathing
- Relaxation breathing exercises
Manual therapy:
- Soft tissue massage of structures that can become tight as a result of apical breathing – diaphragm, chest, neck, upper back around the shoulders and thoracic spine
- Joint mobilisations – stiffness through the ribcage, neck and thoracic spine as a result of altered breathing patterns and movement
Gentle exercise and mobility/stretching
