Temporomandibular Disorder
TMD and TMJ Disorder
What is Temporomandibular disorder?
Temporomandibular disorder (TMD) is the broad term used to describe pain and dysfunction of the
temporomandibular joint (TMJ) and surrounding structures.
The aetiology of TMD is multifactorial and often involves anatomical, pathophysiological and psychosocial factors and there may be a variety of sources contributing to pain or dysfunction including muscular, ligamentous, discal, articular joint, myofascial and neural.
TMD signs and symptoms are estimated to effect 60-70% of the population with those between the ages of 20-40 most commonly effected and women more likely to experience TMD compared to men.
The TMJ is considered one of the most common causes of orofacial pain and is one of the most commonly used joints in the body with direct involvement in actions of mastication (chewing), communication, swallowing and breathing.
Common Causes of TMD
Pain or dysfunction can arise from a number of structures with people most often presenting with a combination of contributing factors
- Changes in the articular cartilage
- Changes in the position or movement of the articular disc
- Change in joint movement
- Muscular changes or imbalances
- Accident or direct trauma
- Cervical spine changes
- Inflammatory disease
Common symptoms associated with TMD
- Localised pain in the jaw
- Restricted movement of the jaw
- Clicking, popping, grating or crepitus
- Headaches
- Tooth pain, twitching eye, numbness in the face, pain behind the eye
- Blocked ear or ear ache
- Sinus problems
- Tinnitus
- Dizziness
- Neck or shoulder pain
TMJ Actions and Roles
The complex joint system, muscles and ligaments allow for the following movements of the TMJ, all of which are essential for those vital tasks including chewing, communication, swallowing and breathing:
- Opening and closing of the mouth
- Protraction of the jaw (forward movement)
- Retraction of the jaw (backward movement)
- Lateral (side-to-side) movement
Anatomy of the TMJ
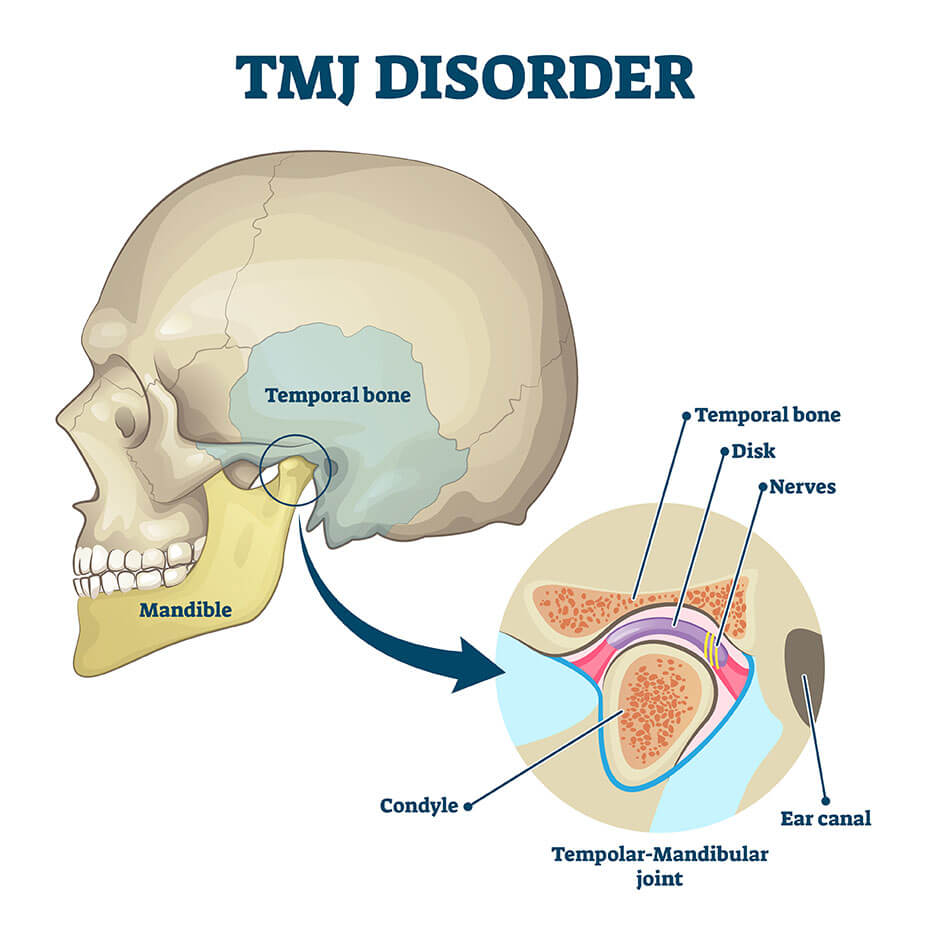
The TMJ is the joint formed by the articulation of the mandibular condyle and the temporal bone. It is a complex synovial joint, classified as a ginglymoarthrodial joint which allows for both rotation and translation movements. Between the two bones of the TMJ (mandible and temporal bones) there is an intra-articular disc which allows for smooth and fluid movement of the joint and helps distribute load over the joint surfaces.The TMJ is unique as it articulates on both sides of the skull which means that movement on one side will affect movement on the other side.
The primary muscles of the TMJ are the masseter, temporalis, suprahyoid and infrahyoid and medial and lateral pterygoid. The main actions of these muscles are opening and closing of the mandible for mastication (chewing) and communication.
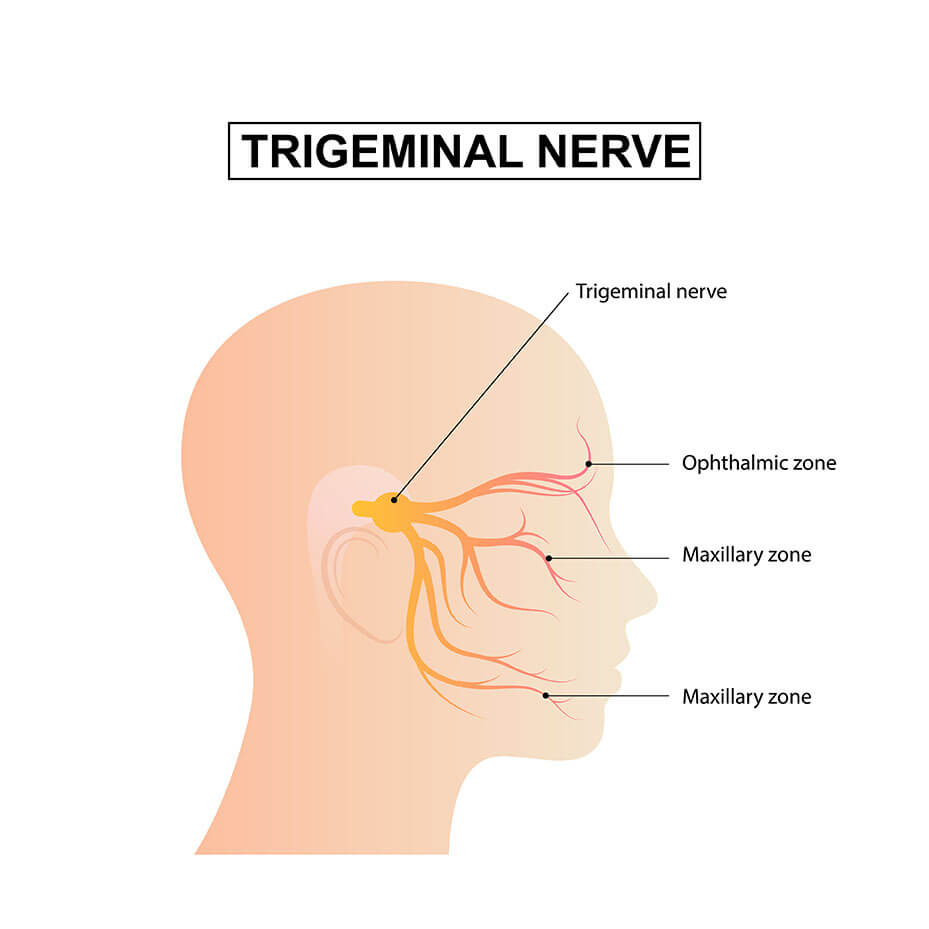
The TMJ is supplied by the mandibular branch of the Trigeminal nerve.
As well as muscles there are numerous ligaments which, along with the joint capsule, assist in controlling movement of the TMJ. These include the temporomandibular ligament, the stylomandibular ligament and the sphenomandibular ligament.
Role of Physiotherapy in TMD
For the majority of people with TMD, conservative management is highly successful in significantly reducing or eliminating symptoms and restoring normal function.
Physiotherapists have a significant role to play in the treatment and management of TMD due to the involvement of muscles, joints, ligaments, myofascial pain and altered biomechanics all of which can be treated through a combination of manual therapy techniques and targeted exercises. Physiotherapists will often form part of a team and work in conjunction with a patient’s dentist, oral surgeon or prosthodontist for more complex TMD presentations. The goal of physiotherapy treatment is to restore joint movement, address muscle imbalances, manage pain and reduce/eliminate mechanical dysfunction.
Physiotherapists will conduct a thorough assessment of the TMJ and surrounding structures including the muscular system, neural system, ligaments and joint biomechanics to determine which components are contributing to pain and dysfunction.
Based upon that assessment, treatment may involve any of the following:
- Correction of posture to improve joint position
- Exercises for the head/neck/eyes/balance/tongue
- External and internal muscle release
- Joint mobilisation
- Myofascial release
- Manual therapy and exercises for the cervical spine, shoulder and upper back
- Acupuncture/dry needling
- Relaxation and breathing techniques
- Pain management techniques
